Overview of Findings
The U.S. Centers for Disease Control and Prevention (CDC) has identified healthMpowerment (HMP) as a good evidence-based intervention (EBI) for HIV risk reduction. Good EBIs are scientifically sound and provide sufficient evidence of efficacy.1 Good EBIs offer promising evidence because they have demonstrated significant positive pre-post intervention differences in 1-group study designs. The CDC recommends health departments and community-based organizations implement evidence-based interventions. The dissemination of risk reduction EBIs is a critical part of building capacity among organizations that implement prevention programs for populations at risk for HIV.2 View the CDC’s description of HMP in their compendium here.

Reductions in Condomless Anal Intercourse
HMP has effectively reduced condomless anal intercourse (CAI) and HIV-related stigma among young Black men who have sex with men (YBMSM) living with and at-risk for HIV. HMP 1.0 was tested in a statewide randomized controlled trial (RCT) in North Carolina with 474 Black men who have sex with men (MSM) aged 18-30 and found statistically significant reductions in CAI.

More Effective When Used 60+ Minutes
The intervention was more effective for participants who used HMP for more than 60 minutes during the 3-month intervention period.

Improved HIV Care Outcomes
In subsequent mixed-methods analysis, online discussions around HIV stigma were associated with HIV-related communication (e.g., provider communication, HIV status disclosure to sexual partners) and improved HIV care outcomes (e.g., perceived barriers to treatment access, engagement in care, self-reported adherence) over time.
History of HealthMpowerment
HealthMpowerment (HMP) 1.0 began development in 2004, in response to a significant percentage of men in North Carolina who are living with HIV and who have sex with men reporting meeting sex partners over the internet.
In 2009, HMP 1.0 enrolled 50 young Black men who have sex with men who were randomized to the HMP website or to a list of currently available HIV/STI websites.
Outcomes for HMP 1.0

Primary Outcome
High levels of user satisfaction and interest and low levels of website difficulty and frustration
Secondary Outcome
A trend in greater behavioral intentions to use condoms and engage in preparatory condom use behaviors in the intervention group (p 0.10)
Secondary Outcome
A reduction in mean scores on the CES-D scale among those in the intervention group (not statistically significant)
Suggestions for Improvement
“Make it structured in a way that people feel empowered to DO SOMETHING.“
More interactions with other users.
Blogs or forum for people wit HIV or STIs to talk about what they are going through and talk with other users on the site.
Games. “It would be neat if scores and usernames could be posted too. Or if there could be a way that we play against other players”
#1 Suggestion
MAKE IT MOBILE
HealthMpowerment Mobile
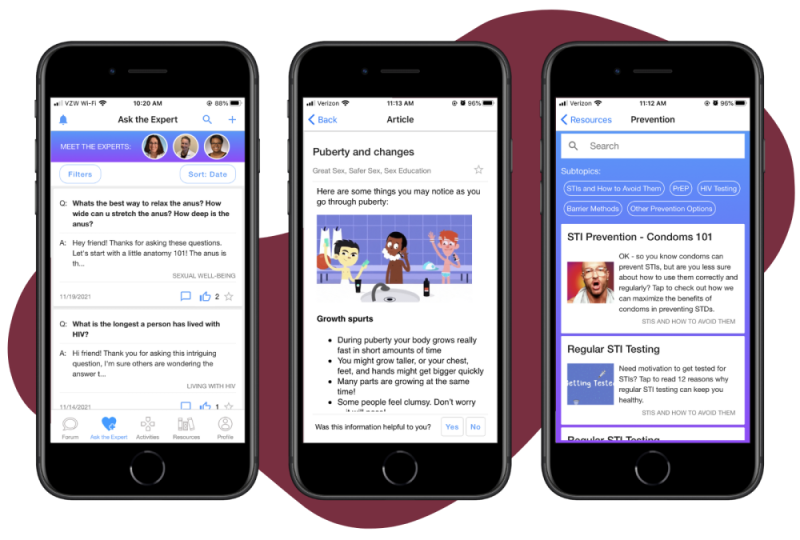
In 2013, we launched a trial for a mobile phone optimized, online intervention for young Black men who have sex with men (YBMSM) aged 18-30, designed to reduce risky sexual behaviors and promote health and wellness. The mobile app was based on behavior change theories and incorporated gamification principles to drive participation and engagement.
The research study built community networks by including peer support based on shared experiences, reinforcing positive behavioral norms, reducing social isolation, and bringing together YBMSM.
The forum was the most popular feature; topics included HIV testing, STI testing, dealing with depression, and HIV medications. The next most popular feature was Ask Dr. W. Participants described the reward elements of exceeding their previous scores and earning points toward prizes as highly motivating.
A 4-week field trial with 15 YBMSM and transgender women found that there were significant improvements in social support (p=0.012), reduction in social isolation (p=0.050) and depression (p=0.045).
The randomized controlled trial (RCT) enrolled 474 YBMSM and transgender women with high risk sexual activity within 6 months of screening. At baseline, 40% were living with HIV, 56% were not living with HIV, and 4% didn’t know their status. The RCT found statistically significant reductions in condomless anal intercourse.
HMP group (IR 0.68, 95% CI: 0.43, 0.93) and the intervention was more effective for participants who used HMP for more than 60 minutes during the 3-month intervention period.
In subsequent mixed-methods analysis, online discussions around HIV stigma were associated with HIV-related communication (e.g., provider communication, HIV status disclosure to sexual partners) and improved HIV care outcomes (e.g., perceived barriers to treatment access, engagement in care, self-reported adherence) over time.
HMP 2.0
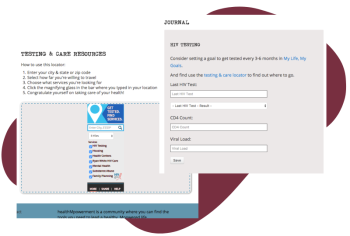
Building upon HMP 1.0, HealthMpowerment 2.0, also known as HMP Stigma, is an app-delivered intervention designed with and for young, Black and Latinx gay, bisexual and other men who have sex with men and transgender women. The intervention aims to improve HIV prevention and care by providing a platform where participants can find social support, build community, and engage with issues that matter to them.
The app includes educational information on a range of health and lifestyle topics, delivered in a variety of formats (e.g. articles, quizzes, activities). HIV testing, prevention, and care resources are provided through an “Ask the Expert” feature hosted by a health navigator and board-certified infectious disease physician. The HMP approach strives to amplify resilience among participants by bringing diverse people together in dialogue as a critical step toward change.